“Depriving yourself is like how a diabetic would feel if they didn’t take their insulin.”
Virginia Skipper said that it wasn’t until her physician made that comparison that she finally understood how serious it was. Medicating for her depression wasn’t this “happy pill.” Everything would not be fixed, but not medicating, and not treating mental health, was physically depriving herself, despite any stigma surrounding it.
Skipper, a recent graduate with a bachelors of science and psychology, didn’t see the signs, even as she went to all her psychology classes, she couldn’t wrap her head around what was happening, why doing mediocre tasks kept getting more and more painful. She didn’t want to go to the doctor, any doctor.
“Freshman year, second semester, I started feeling sad for no reason. I didn’t really know what was going on because it’d never happened to me before. I had no reason to be sad. I was making friends, there was no breakup, no death, no traumatic event. I was just feeling sad,” Skipper said.
She associated it with business and distraction. She told herself to cheer up.
She remembered all the times the depressive episodes got out of control, with her crying, sometimes for long, painful periods of time, every day. Not the cute crying, she said, the choking on snot crying.
For some students, fear and blame rattles around in their brain, constantly in a shame-shocked conflict about how long is too long to ask for help. Only about 11 percent of students reached out to counseling centers when they needed help, according to the National Survey of College Counseling Centers.
She felt like if she told any of her friends or parents, they would look at her differently. She said that a complete stranger was easier to talk to than her best friend.
“The (SHC) counselor was the only one in my life that knew, and that goes to a lot of the stigma,” Skipper said.
She realized she wasn’t connecting to her counselor, so she stopped going.
At first, she would just go running every time the feelings started to bombard her or keep her in bed for an entire day. She almost associated running with the feelings now, how they would lesson but never diminish, pushed away by surges of endorphins. Except for one time she was running, she started to feel really nauseous, terrified and overwhelmed. Eventually, she fainted and woke up alone.
“I went behind a building and sat down, hyperventilating, and I just kind of went out of it and woke up laying down. I couldn’t catch my breath, it was very physical symptoms from a mental illness,” Skipper said. “That’s when I called my mom, I was scared what was happening.”
Skipper knew it was bad.
Depression and anxiety often go hand in hand.
Anxiety disorders are complex and develop from a risk factors such as genetics and brain chemistry, personalities and traumatic life events. Currently, almost one-half of people diagnosed with depression are also diagnosed with an anxiety disorder or vice versa, according to the Anxiety and Depression Association of America.
The 2014 National Survey of College Counseling Centers covered 275 schools, with 63 of them counted in the biggest category of student populations, including The University of Alabama. The survey was completed by college counselors and psychiatric professionals on each campus. When all the schools were asked about changes in student depression and anxiety over the last five years, the answers were clear-cut.
For every category, zero percent of professionals thought the amount of students with anxiety or depression on campus was decreasing. Young professionals, especially when going to college and completely changing their lifestyle, seem to be at increased risk for mental illness.
After Skipper took a depression questionnaire, her doctor told her that she was depressed and suggested medicine.
In 18 to 25-year-olds, anti-depressants affects the chemistry in their brain, which worried Skipper. Her doctor said it takes until that age for the brain to finish developing. It’s a medicine to stabilize the chemistry that’s a little bit off.
“That’s what makes it so difficult to catch. People expect you to change when you’re that age,” AnneRea Gwarjanski, who suffers from severe depression and studies mental illness said, exasperated. “That’s the age of adulthood. You’re finally supposed to stand on your own but –you need help.”
Eradicating the stigma, Gwarjanski realized, hasn’t been and isn’t going to be easy.
“I feel like there’s a hierarchy in stigmatized mental illness, and the depression stigma is more so that you’re just sad and blue and you’ll snap out of it. I felt like people would perceive me as weak and vain,” she said, and that’s why for a long time, she didn’t tell anyone.
She’s not the only student that felt that way.
When UA student Rachael Chudoba, a senior majoring in restaurant and hospitality management, looked back at her experience with mental health, she wished she would have thought twice, asked for another opinion instead of taking her doctor’s word as the sole authority of how she felt.
The symptoms started for her in her senior year of high school, and when freshman year of college rolled around, they only got worse. After going through her first year of college untreated, she went to her doctor and he prescribed her with Zoloft, a common medicine used to treat anxiety and depression.
Driving home from the appointments, she felt defeated every time. The questions were general and surface level and she wasn’t realizing anything new or getting anywhere. People kept telling her she seemed so happy, but being an outgoing person doesn’t mean you can’t experience depression and anxiety. She went shopping and got manicures. She ate late-night Easy Mac. She kept going to classes, showing up all the parties, visiting home, laughing with all her sorority sisters, trucking through “the daily life” just like her friends expected.
It was internal, and that’s how she kept it. The Zoloft dulled it all into motions.
“When it didn’t [help], I went through this self doubt, like ‘maybe this is my personality’ and ‘maybe I should just learn to deal with this,’ ” she said.
Eventually, she decided to do her own online research instead of going back to the doctor for the same experience.
“That’s how it was like at the Student Health Center, They kind of just said ‘here you go, this will help,’ and when it didn’t, they would just bump me up a milligram, go to 150, ” Chudoba said. “I’m still sad. Bump me up to 250, I’m still sad. Bump me up.,
When her doctor recommended getting therapy from UA professionals at the Counseling Center, she felt uneasy. It was definitely too serious for her problems. It would be silly; there was no way her problems were that important, plus, she just upped her medicine, so that would cover it. Backed with a huge support group of friends, she had people to talk to, and this way she didn’t have to risk seeing someone from her classes. The idea was dismissed.
“For me, it felt too invasive for a college campus.”
Unlike, Chudoba, eighty-six percent of counseling center directors report that there has been a steady increase in the number of students arriving on campus already on psychiatric medication, according to the study that include The University of Alabama. Usually medicine is paired with counseling, but if students are already on medicine, they don’t always feel the need to go get help. Some students don’t want to go either way.
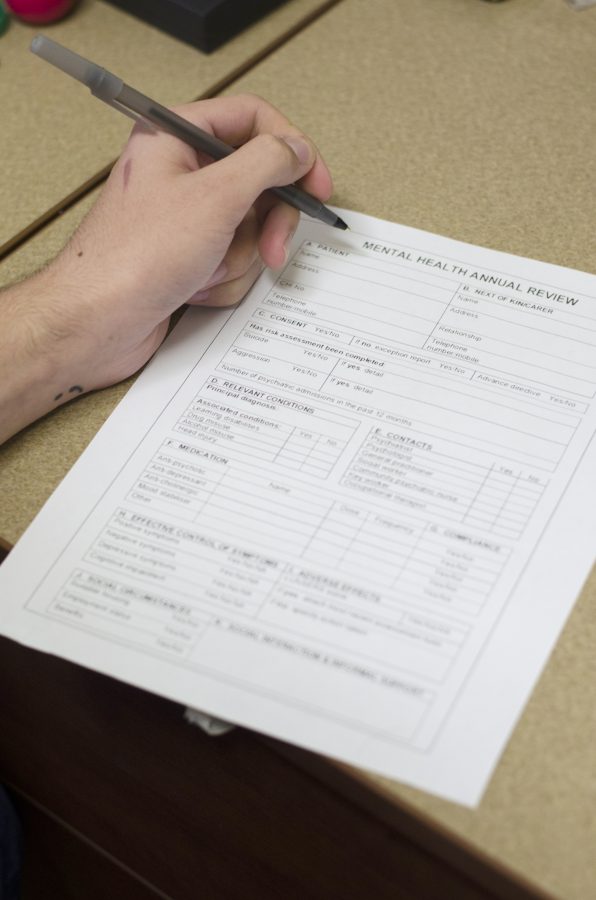
The UA Counseling center helps students “achieve academic success and personal growth through quality brief counseling,” according to its website. Services for students are confidential, as long as they are within legal guidelines, but the sessions are limited to 15 per academic year, so it’s not suitable for combatting mental health long-term combat.
Professional therapists have also been effective for many students, especially if they are uneasy about implementing medicine.
“You and I can talk, and you can sympathize, but you don’t understand what I’m going through,” said Caroline Gazzara, a senior majoring in journalism. “I talk, [therapists] they understand the mechanics of what I’m thinking. They’re not going to say ‘I’m sorry,’ they’re actually going to take the sadness and make it something good.”
Anti-depressant pills, which usually effectively also treat anxiety, aren’t for everyone.
For Gazzara, it wasn’t medically an option. When her doctor recommended that she go on anti-depressants to help curtail the depression and anxiety that followed being hit by a car freshman year, they quickly realized that if she took the medicine, it would cause dysfunctionality in the pain medicine for her back. Relief from the daily physical pain made her life bearable. After the accident, she spent the next year either in bed, a redhibitory program or intensive physical therapy, but always prescribed to multiple powerful pain relievers.
“I wake up, I hurt and I remember everything,” Gazzara said, explaining that with her parents being so far away, they thought that she was alright. “I’m the one who went and saw someone when my mom said ‘you don’t need anyone.’ ”
Her mom knew Gazzara was strong, she just had to warm up to the idea of therapy. She waited a year before seeking out a therapist from the UA Counseling Center.
Her boyfriend also cheated on her at the time and blamed her for the accident. It all started to pile up. The depression just wouldn’t go away.
“I kept, just, internally compressing everything, and blaming myself. I know it’s not my fault; I just couldn’t accept anything,” she said.
Each session, she cried, and even though she’d been put in therapy after moving when she was a lot younger, it was disappointing when she didn’t “click” or connect with the first counselor. Gazzaba was willing to pay the cost of $15 per session after the first visit. She said that it was reasonably priced compared to most off-campus therapy sessions. The bills can also be sent to a different account then the parent’s account.
Both Chudoba and Gazzaba were successful looking beyond medication.
Chudoba no longer visits the doctor or takes any medication, and she credits this to a singular commitment: lifestyle changes.
She changed her diet, took out processed foods, went to all natural products in her household and started exercising regularly. She doesn’t eat dairy for the most part and has taken her caffeine consumption way down. She made wellness a part of her routine and realized along the way that these were some of the things that truly made her happy. They sparked joy.
Chudoba explained she wasn’t structuring her life in a really strict way, she was just learning what worked.
Now she learned to take time out of her day, every day, no matter what, to just do something not on her todo list. Some days it’s meditating, or painting, or something that just completely wastes time.
For Chudoba, it took a lot of changes. She had to get to know her body, what it needed, and her mind and what made her happy. It’s a topic she’s passionate about. She laughed because sometimes people say she sounds like a hippy, but they don’t know what it’s like for her to be able to remember her depression and anxiety as a thing of the past.
“It’s an investment in your health. It’s important,” she said.
Personally, Gazzaba loved her therapy experience. It pushed her for closure.
Gazzaba was sick of not feelings like herself; she wanted to date again, meet people, volunteer to do things people asked from her. She was sick of feeling scared, of the recurring nightmares and that heavy, constant feeling of being a useless human being.
If she feels like she’s about to have a panic attack, she takes passion flower, an alternative medicine sold at Mana Grocery. It calms her if the holy basil she takes twice a day to regulate her anxiety doesn’t. She even took a UA class dedicated entirely alternative medicine. She she still does some of the breathing exercises she learned, and she’s not afraid to make another counseling appointment if she get too overwhelmed, or needs a mental health check.
“That’s how that anxiety snowball works,” Chudoba said. “You’re surrounded by it, then you start thinking like that, then acting like that.”
Then, she said, you have to cut it off at the source.
Telling someone, be it a friend or counselor, is the start of that. Often, if the anxiety and depressions continues to build and build, struggling students began to see predominately physical consequences.
This surprised many students, including Skipper.
“I’m not the kind of person to admit that I need help, but I had to,” she said.
Gwarjanski, who fought hard and long to avoid seeking help, said she knows what it’s like to be that stubborn, to the point where it seriously affected her life. Eating disorders often pair with severe depression, and when Gwarjanski became bulimic when she was 17 years old and on the swim team, the feeling that her life didn’t matter became hard to shake. She couldn’t tell anyone–she felt too dramatic, she felt like it must not be real.
Now she said that it shows more strength to seek help than it does to hide.
Even though she admits, along with Skipper, that some days are still incredibly painful, and it feels impossible to even do the most mediocre things, she’s seen that getting your body at a healthy level, as well as communicating against the stigma, is what helped her most on those days.
“You’re taught the kind of ‘pull yourself up by the bootstraps’ kind of narrative,” Gwarjanski said. “Except really, they [therapists] want to help you, but you have to ask. That part is on you.”
With her graduate thesis being about mental health and stigmas, she said that there’s been a lot of research that the news media does not give accurate, full information and that they sometimes mislead the public on mental illness.
“People look down at millennials a lot, they say we are too sensitive, we get offended easily but really I think we know better, and we got to do better,” she said.
She said you have to realize that people go through different struggles, and she is surprised at how much empathy she now has. But also, she said that people have the opportunities to treat themselves with resources these days.
Now, Skipper said that her depressive episodes are further and fewer in between, and she sees her primary care physician regularly. For Skipper, she is one of the people she truly trusts, which she knew was not what everyone felt like with their doctors or therapists. Gwarjanski felt the same way. She absolutely loved her doctor, and even followed her to another practice.
When she posted a blog post on her mental health experiences, she was surprised by the honest, powerful support from so many different people. Even though she also has gone off medication, she said that combined with lifestyle changes, it can make the difference.
“It was scary to think that this was a drug that was going to change my brain chemistry,” Gwasjanski said. “Actually, it allowed me to still be curious, silly, competitive and toned down my normal emotions.”
At least she knew she wasn’t alone.